News
Pain management in FSHD

Chronic pain is one of the more difficult aspects of living with FSHD, and also one of the most challenging to manage.
In various studies, between 82 and 89 percent of people with FSHD reported having significant pain, with 19 percent rating their pain level as “severe.” In this video from our FSHD University webinar, neurologist Kathy Mathews, psychologist Krista Kohl, and physical therapist Shelley Mockler explain that multiple factors go into an individual’s experience of pain. Consequently, they say that patients and their healthcare team need to develop a multi-pronged strategy to manage pain.
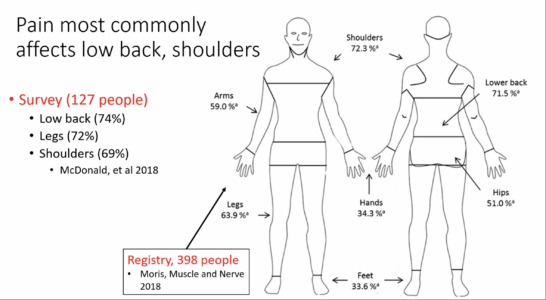
People report pain in many areas of the body, most frequently in the shoulders and lower back. There’s no single source or type of pain, and the level of pain bears no relationship with disease severity, age, or genetics.
Dr. Mathews advises individuals seeing a pain specialist to “describe the pain in as much detail as you can. What makes it better or worse? When does it occur?” She emphasized that “pain is experienced in the brain,” and that this is a very important principle because “you can’t treat pain without involving the brain.” This by no means implies that pain is “all in the head,” but that focusing solely on the aching body part is often not sufficient, especially in chronic pain.
Dr. Kohl described the biopsychosocial model of pain, which involves linkages between chronic pain with such symptoms as depression, anxiety, and post-traumatic stress disorder. Pain can interfere with sleep, which in turn sets off a negative feedback cycle of fatigue, mood, activity, and energy. Understanding these links can help identify ways to intervene, she said.
The team emphasized that the treatment of chronic pain is most successful when you use multiple approaches. This image of “What’s in your cup” suggests some key contributors to pain–and ways to address them. How can you build a bigger cup to be able to manage pain? Can you change your environment to remove pain triggers or reduce painful movements?
Remedies such as exercise, massage, electrical stimulation, foam rollers, and medications, provide relief that is short-term, but that may be enough to help re-set the negative feedback loops. A good physical therapist can be a key ally. “Think of your PT as a coach, not as someone who will ‘fix your pain,'” counseled Shelley Mockler. “Look for someone willing to learn.”
Here you will find further materials and information to learn more.
To stay up to date on FSHD Society activities, you can fill out this form and join the community!
The form is also accessible from the QR Code below.